Many Mental Health Disorders list genetics or family history among their risk factors. While this might not seem out of the ordinary—after all, plenty of diseases that run in families—there can be confusion over how genetics affect mental health.
This is particularly true for Depressive Disorders, which are among the most common Mental Health Disorders in adults. If Depression runs in your family, are you going to develop a Depressive Disorder? How likely are you to develop a Depressive Disorder because of your family history?
Unfortunately, there is no hard and fast rule; both genetics and Mental Health Conditions affect everyone differently. But learning about the role genetics plays in Depression diagnosis can help you understand your own causes and risk factors. Explore the ins and outs of genetics, other Depressive Disorder risk factors, and how these factors affect your own experience with Mental Health Disorders with this guide.
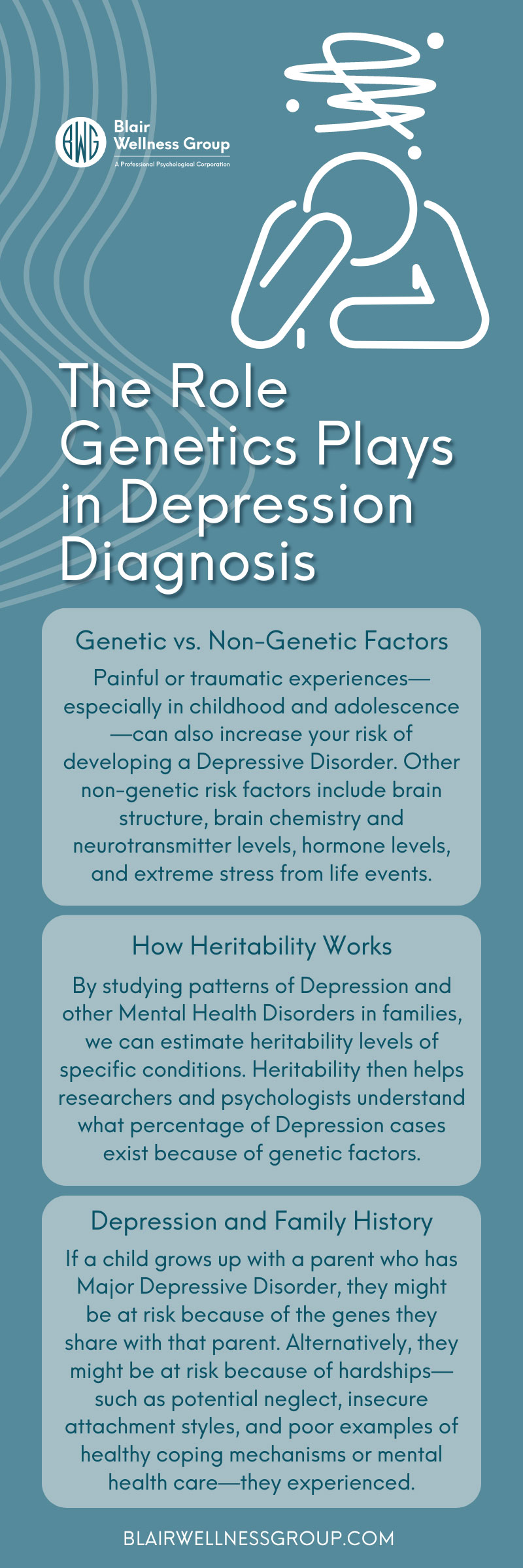
Genetic vs. Non-Genetic Factors
Genetics are far from the only factor that can cause Depressive Disorders. You must also have a firm understanding of the effects of non-genetic factors to fairly discuss the influence of genetic factors. For example, painful or traumatic experiences—especially in childhood and adolescence—can also increase your risk of developing a Depressive Disorder. Other non-genetic risk factors include brain structure, brain chemistry and neurotransmitter levels, hormone levels, and extreme stress from life events.
Why is it important to learn about non-genetic factors? Genetic factors can closely intertwine with physical or psychological risk factors, which introduces the question of nature versus nurture. Does a child with a genetic predisposition to Major Depressive Disorder develop the condition because their parent has it? Or do they develop the condition because they grew up learning the poor behaviors, thought patterns, and emotional regulation skills of a guardian figure with Depression? Both situations are possible.
How Heritability Works
Scientists are still learning more about how genetics cause Depressive Disorders. By studying patterns of Depression and other Mental Health Disorders in families, we can estimate heritability levels of specific conditions. Heritability then helps researchers and psychologists understand what percentage of Depression cases exist because of genetic factors.
Most estimates state that heritability for Depression is around 50 percent, but that number might be higher for severe Depressive Disorders. However, it is difficult to say whether that means genes play a role in roughly half of the Depressive Disorder cases or if that probability changes on a case-by-case basis. It could be that one individual might solely have a genetic risk factor while another individual might only have non-genetic risk factors for a Depressive Disorder.
Depression and Family History
Generally speaking, individuals with family members who have had a Depressive Disorder are at greater risk of developing the disorder themselves. That risk increases when said family members experience a severe Depressive Disorder or have reoccurring cases of Depression. The risk factor also increases if the Depressive Disorder occurs early on in life.
However, there is still a question of whether that increased risk is purely genetic. If a child grows up with a parent who has Major Depressive Disorder, they might be at risk because of the genes they share with that parent. Alternatively, they might be at risk because of hardships—such as potential neglect, insecure attachment styles, and poor examples of healthy coping mechanisms or mental health care—they experienced.
Predisposition Is Not Direct Inheritance
It is important to note the difference between genetic predisposition and inheriting a so-called “depression gene.” Even with a higher chance of heritability, you are not directly inheriting a Depressive Disorder from a parent or other family member. Unlike disorders such as cystic fibrosis or Huntington’s disease, Depression does not come from a single defective gene. Instead, there are a handful of different genetic combinations that make developing a Depressive Disorder more likely.
As such, you are not inheriting your Depression from a family member. You are simply inheriting a combination of genes that run in your family, some of which might create a predisposition to Depressive Disorders.
Genetic Predisposition and Comorbid Disorders
Depressive Disorder has high rates of comorbidity with other Mental Health Disorders. Some of the most common disorders that are comorbid with Depression include Anxiety Disorders, Drug and Substance Abuse, Alcohol Addiction, and Personality Disorders.
As with many Mental Health Disorders, developing a comorbid disorder is not necessarily genetic. Other factors—such as unhealthy coping mechanisms leading to Addiction Disorders—might lead to the development of a comorbid condition. However, certain genetic combinations might still play a role in comorbid disorders.
For example, a genetic predisposition to Major Depressive Disorder can increase your chances of developing Depression and a comorbid Anxiety Disorder. This is also true in reverse: a genetic disposition to General Anxiety Disorder can increase your chances of developing a comorbid Depressive Disorder.
Genetics and Depression Diagnosis
Whether your Depressive Disorder stems from a genetic predisposition or non-genetic factors, it does not influence the potential symptoms you might face. As such, the role that genetics plays in Depression diagnosis does not affect the signs and symptoms of Depression that will tell you it is time to seek help. No matter what causes your Depression, you might still face the following physical, mental, and emotional symptoms.
- Fatigue, exhaustion, and a lack of energy
- Insomnia
- Excessive sleeping
- Feelings of hopelessness
- Feelings of guilt or worthlessness
- Feelings of frustration or irritability
- Loss of interest in hobbies, social activities, and other things you once
- enjoyed
- Changes in appetite
- Significant and unexpected weight changes
- Headaches, cramps, or body aches
A family history of Depressive Disorders might make you aware of the common indicators of Depression, which can make it easier to seek professional treatment once you recognize symptoms. Conversely, that same family history might normalize symptoms of Depression, causing you to accept these indicators as natural and avoid seeking mental health treatment. Knowing the common symptoms of Depression and understanding the importance of seeking professional help is crucial for your mental, emotional, and physical well-being—no matter what caused your Depressive Disorder.
Professional Treatment Helps
Professional, evidence-based treatment from a Licensed Clinical Psychologist helps you overcome the symptoms and challenges of Depressive Disorders regardless of whether genetics play a role. If you are looking for expert Depression treatment in Newport Beach, turn to the team at Blair Wellness Group. Work with our team to set up an appointment and pursue an effective, lasting treatment plan that is right for you and your unique experience with mental health.